Image copyrightAP
Image copyrightAPThe hunt for a cancer cure should be treated with as much urgency as the Ebola outbreak, says US Vice-President Joe Biden.
He said he had dreamed of being the president that cured cancer and believed it was possible.
He is now leading the US “cancer moonshot” programme to cure cancer.
He told scientists their success could “literally change the world” but criticised the barriers to getting on clinical trials.
In a speech to American Society of Clinical Oncology annual meeting he said: “[When] we were worried about Ebola we were able to aggregate tens of millions of dollars and the entire US military because the World Health Organization couldn’t handle it.
“That’s the kind of urgency we need with regard to cancer.”
In January, President Barack Obama announced the $1bn (£710m) “moonshot” and that Joe Biden would lead it.
The vice-president said: “If I could have done anything I would have wanted to be the president that ended cancer as we know it because I believe it is now possible.”
It is a personal mission for Mr Biden, who lost his son Beau to brain cancer at the age of 46 last year.
He told the meeting of 30,000 of the world’s leading cancer scientists and doctors that his son had been able to take part in pioneering clinical trials.
But “what about the 96% of people” who miss out, he asked, and called for new measures to help the poorest patients take part.
“Nobody should have to forgo a critical clinical trial because they cannot afford the gas to get there or a baby sitter at home,” he said.
His speech referenced many of the major themes that have emerged at the meeting in Chicago including the transformative power of immunotherapy and the unparalleled understanding of the genetics of cancer.
“[They are] offering profound promise that wasn’t there five years ago,” he said.
But Mr Biden said the progress could be much faster if only scientists worked closely together.
He said: “Imagine if we all worked together… shared the data behind breakthroughs so that the field as a whole can move forward faster and avoid unnecessary redundancy.
“The whole world is looking to you, your success can literally change the world. We need you now more than we ever have.”
Huge breakthroughs
Dr Deborah Mayer, one of the expert advisers to the moonshot, said there had been terrific progress in cancer science and the field was now at a “tipping point”.
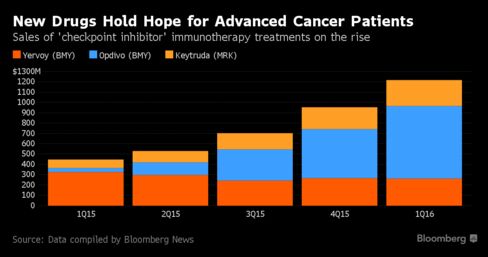
Huge breakthroughs in harnessing the power of the immune system to attack tumours or in tailoring drugs to the weak spot in individual patients’ tumours are already helping patients.
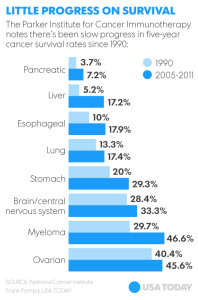
In the US, five-year cancer survival has increased from 30% in 1950 to 48% in 1975 and 68% in 2010.
Dr Mayer told the BBC News website that the moonshot would act as a catalyst to bring breakthroughs to patients faster.
“Hopefully it will close that 17-year gap between what we know and what we do.
“The benefit to patients of this moonshot is we will move forward to enhanced treatments, we’re going to find cancers earlier when they’re more curable and we’re going to figure out how to prevent them.”
The American Society of Clinical Oncology has recommended four key areas the moonshot needs to deal with.
- Shortening the time needed to perform trials and bring drugs to market
- Developing tests that show which targeted therapies will benefit patients
- Increasing data sharing between companies, researchers and hospitals
- Boosting collaboration in the cancer field
The organisation’s president Dr Julie Vose said: “The Moonshot Initiative can be a vehicle for major new progress against cancer.”